Nutrition UNIT 3 NUTRITION FOR INFANT, CHILD,
ADOLESCENT AND ELDERLY
Structure
3.0 Introduction
3.1 Objectives
3.2 Significance of Nutrition across Life Cycle
3.3 Infant and Young Child Feeding (IYCF)
3.3.1 First Food for the Baby
3.3.2 Traditional Foods for Infants
3.3.3 Modified Family Food
3.3.4 Instant Infant Foods
3.3.5 Protective Foods
3.3.6 Energy Density of Infant Foods
3.3.7 Frequency of Feeding
3.3.8 Continued Breastfeeding
3.3.9 Active Feeding
3.4 Nutritional needs of Children and Adolescents
3.5 Nutritional needs of Pregnant and Lactating Mothers
3.5.1 Nutrition of Pregnant Women
3.5.2 Nutrition of Lactating Mothers
3.6 Nutritional needs for the Elderly
3.7 Important National Nutritional Programmes
3.7.1 Integrated Child Development Services (ICDS) Scheme
3.7.2 National Programme of Mid Day Meal in Schools (MDMS)
3.8 Let Us Sum Up
3.9 Model Answers
3.10 References
3.0 INTRODUCTION
In Unit 2 you have learnt about importance of nutrition during pregnancy and
lactation.
Good nutrition is the key to well-being of humans and lays the base for healthy
life. It is a fundamental to achieving positive health, functional efficiency and
productivity. The nutritional needs of the human body change across the lifecycle.
For any given individual, the requirement of nutrients is dependent on his/her
age, physiological status, physical activity, Basal Metabolic Rate (BMR) etc.
Nutritional status is internationally recognised as an indicator of national
development. Malnutrition, which encompasses both under-nutrition as well as
over-nutrition, is recognised as an important public health problem and is one of
the toughest challenges that the global community is facing today.
In this unit we shall discusses the nutritional requirements across the lifecycle
and how to meet that changed requirement through balanced diet.
Nutrition for Infant, Child, 3.1 OBJECTIVES Adolescent and Elderly
After completing this unit, you shall be able to:
• know the Infant and Young Child Feeding (IYCF) guidelines;
• explain the nutritional needs of children, adolescents and elderly; and
• describe important National Nutritional Programmes.
3.2 SIGNIFICANCE OF NUTRITION ACROSS
LIFE CYCLE
• Globally 45% of all child deaths are attributed to underweight.
• The magnitude of child under-nutrition in India is one of the highest in the
world. Around 39 per cent of under 5 children in India are stunted, 15 per
cent are wasted and 29 per cent are underweight with every sixth child in
India being severely stunted, one in 20 being severely wasted and one in ten
child being severely underweight.
• About 55% men and 75% non pregnant non lactating women are anaemic.
• Under nutrition during foetal and early childhood is known to be associated
with chronic diseases in later life.
• Chronic diseases like coronary artery disease, hypertension, type 2 diabetes,
some cancers are related to diet and nutritional status.
• Obesity is associated with higher risk of developing cancer breast, colon,
endometrium, gallbladder, oesophagus, pancreas, etc.
• Consumption of foods rich in dietary fiber and antioxidants is associated
with reduced risk of certain cancers.
3.3 INFANT AND YOUNG CHILD FEEDING
GUIDELINES
Infant and Young Child Feeding (IYCF) is a set of well-known and common
recommendations for appropriate feeding of new-born and children under two
years of age. IYCF includes the following care practices.
Early Initiation of Breastfeeding means breastfeeding all normal newborns
(including those born by caesarean section) as early as possible after birth, ideally
within first hour. Colostrum, the milk secreted in the first 2–3 days, must not be
discarded but should be fed to newborn as it contains high concentration of
protective immunoglobulin’s and cells. No pre-lacteal fluid should be given to
the newborn.
Colostrum contains large quantities of protective substances and growth factors
and has more protein and Vitamins A and K than mature milk. It enhances the
development and maturation of the baby’s gastro-intestinal tract. The anti-infective
proteins and white cells provide the first immunisation against the diseases that
a baby encounters after delivery. Although colostrum is secreted in small quantities
(30–90 ml), it is sufficient to meet the caloric needs of a normal newborn in the
first few days of life. Colostrum also has a mild purgative effect, which helps to
66
Nutrition clear baby’s gut of meconium (the first, very dark stools) and helps to prevent
jaundice by clearing the bilirubin from the gut. It stimulates the baby’s immature
intestine to develop in order to digest and absorb milk and to prevent the absorption
of undigested protein.
Exclusive breastfeeding for the first 6 months means that an infant receives only
breast milk from his or her mother or a wet nurse, or expressed breast milk, and
no other liquids or solids, not even water. The only exceptions include
administration of oral rehydration solution, oral vaccines, vitamins, minerals
supplements or medicines.
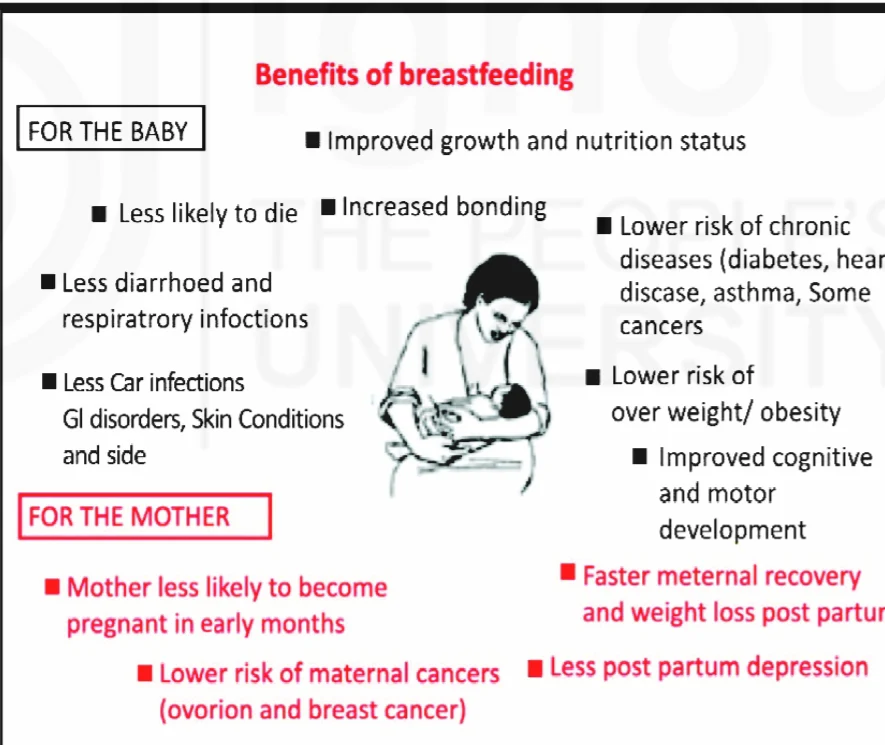
Following are the advantages of breastfeeding, breast milk is:
the best natural food for babies.
always clean.
protects the baby from diseases.
makes the child more intelligent.
available 24 hours a day and requires no special preparation.
nature’s gift to the infant and does not need to be purchased.
Breastfeeding makes a special relationship between mother and baby, helps
parents to space their children, and helps mother to shed extra-weight gained
during pregnancy.
Fig. 3.1: Benefits of Breastfeeding
Complementary feeding means complementing solid/semi-solid food with breast
milk after child attains age of six months. After the age of 6 months, breast milk
is no longer sufficient to meet the nutritional requirements of infants. However
infants are vulnerable during the transition, from exclusive breast milk to the
introduction of complementary feeding, over and above the breast milk. For
Nutrition for Infant, Child,
Adolescent and Elderly
ensuring that the nutritional needs of a young child are met breastfeeding must
continue along with appropriate complementary feeding. The term
“complementary feeding” and not “weaning” should be used. The complementary
feeding must be:
Timely - meaning that they are introduced when the need for energy and
nutrients exceeds what can be provided through exclusive breastfeeding.
Adequate - meaning that they provide sufficient energy, protein and micro-
nutrients to meet a growing child’s nutritional needs.
Safe - meaning the food is hygienically prepared, stored and fed with clean
hands using clean utensils instead of bottles and/or teats.
Active feeding - styles for complementary feeding are also important.
Appropriate feeding styles can provide significant learning opportunities
through responsive caregiver interaction, enhancing brain development in
the most crucial first three years.
Fig. 3.2: Benefits of Optimal Complementary Feeding
3.3.1 First Food for the Baby
The staple cereal of the family should be used to make the first food for an infant.
Porridge can be made with suji (semolina), broken wheat, atta (wheat flour) ground
rice, ragi, millet etc, by using a little water or milk, if available. Roasted flour of
any cereal can be mixed with boiled water, sugar and a little fat to make the first
complementary food for the baby and could be started on the day the child becomes
six months old. Adding sugar or jaggery and ghee or oil is important as it increases
the energy value of the food. In the beginning the porridge could be made a little
thinner but as the child grows older the consistency has to be thicker. A thick
porridge is more nutritious than a thin one. In case a family can not prepare the
porridge for the infant separately, pieces of half chapati could be soaked in half a
cup of milk or boiled water, mashed properly and fed to the baby after adding
anaemia
sugar and fat. Soaked and mashed chapatti could be passed through a sieve so as
to get a soft semi-solid food for the infant.
Fruits like banana, papaya, chikoo, mango etc could be given at this age in a
mashed form. Infants could also be given reconstituted instant infant foods
(preparation of which is discussed a little later) at this age.
3.3.2 Traditional Foods for Infants
Once the child is eating the cereal porridge well, mixed foods including cooked
cereal, pulse and vegetable(s) could be given to the child. Most traditional foods
given to infants in different parts of the country are examples of mixed foods
like khichdi, dalia, sujikheer, upma, idli, dokhla, bhaat-bhaji etc. Sometimes
traditional foods are given after a little modification so as to make the food more
suitable for the child. For instance, mashed idli with a little oil and sugar is a
good complementary food for the infant. Similarly bhaat can be made more
nutritious by adding some cooked dal or vegetable to it. Khichdi can be made
more nutritious by adding one or two vegetables in it while cooking.
3.3.3 Modified Family Food
In most families there is a cereal preparation in the form of roti or rice and a
pulse or a vegetable preparation. For preparing a complementary food for the
infant from the foods cooked for the family, a small amount of dal or vegetable
preparation should be separated before adding spices to it. Pieces of chapati could
be soaked in half a katori of dal and some vegetable, if available. The mixed food
could be mashed well and fed to the baby after adding a little oil. If necessary the
mixture could be passed through a sieve to get a semi-solid paste. Thus, rice or
wheat preparation could be mixed with pulse and/or vegetable to make a nutritious
complementary food for the infant. Modifying family’s food is one of the most
effective ways of ensuring complementary feeding of infants.
3.3.4 Instant Infant Foods
Infant food mixes can be made at home from food grains available in the
household. These mixes can be stored atleast for a month and enable frequent
feeding of infants. These are sattu like preparations which is quite familiar in the
Indian community. One can take three parts of any cereal (rice/wheat) or millet
(ragi, bajra, jowar), one part of any pulse (moong/channa/arhar) and half part of
groundnuts or white til, if available. The food items should be roasted separately,
ground, mixed properly and stored in airtight containers. For feeding, take two
tablespoons of this infant food mix, add boiled hot water or milk, sugar or jaggery
and oil/ghee and mix well. Cooked and mashed carrot, pumpkin or green leafy
vegetables could be added to the porridge, if available. The infant can be fed
with this food whenever freshly cookedfood is not available in the family. The
infant food mix could also be made into preparations like halwa, burfi, upma,
dalia etc, and given to the child.
3.3.5 Protective Foods
Besides modified family food and reconstituted infant food mixes, protective
foods like milk, curd, lassi, egg, fish and fruits and vegetables are also important
to help in the healthy growth of the infants. Green leafy vegetables, carrots,
pumpkin and seasonal fruits like papaya, mango, chikoo, banana etc., are
important to ensure good vitamin A and iron status of the child. Baby needs all
foods from six months namely cereals, pulses, vegetables particularly green
leafy vegetables, fruits, milk and milk products, egg, meat and fish if non-
vegetarian, oil/ghee, sugar and iodised salt in addition to breastfeeding. A
diversified diet of the infant alongwith breastfeeding will also improve the
micronutrients’ status of the child.
3.3.6 Energy Density of Infant Foods
Low energy density of complementary foods given to young children and low
frequency of feeding result in inadequate calorie intake and thus the
malnutrition. Most of the foods are bulky and a child cannot eat more at
a time. Hence it is important to give small energy dense feeds at frequent
intervals to the child with a view to ensure adequate energy intake by the
child. Energy density of foods given to infants and young children can be
increased in four different ways:
i) By adding a teaspoonful of oil or ghee in every feed. Fat is a concentrated
source of energy and substantially increases energy content of food without
increasing the bulk. The false belief in the community that a young child
cannot digest fat has to be dispelled with by informing that a young infant
digests fat present in breast milk and all other foods like cereals and pulses
and that there is no reason to feel that a child can not digest visible fat when
added to food.
ii) By adding sugar or jaggery to the child’s food. Children need more
energy and hence adequate amounts of sugar or jaggery should be added
to child’s food.
iii) By giving malted foods. Malting reduces viscosity of the foods and hence
child can eat more at a time. Malting is germinating whole grain cereal or
pulse, drying it after germination and grinding. Infant Food Mixes prepared
after malting the cereal or pulse will provide more energy to the child. Flours
of malted food when mixed with other foods help in reducing the viscosity
of that food. Amylase Rich Flour (ARF) is the scientific name given to
flours of malted foods and must be utilised in infant foods.
iv) By feeding thick mixtures. Thin gruels do not provide enough energy. A
young infant particularly during 6–9 months requires thick but smooth
mixtures as hard pieces in the semi-solid food may cause difficulty if
swallowed. The semi-solid foods for young infants can be passed through a
sieve by pressing with a ladle to ensure that the mixed food is smooth and
uniform without any big pieces or lumps.
3.3.7 Frequency of Feeding
Infants and young children need to be fed 5–6 times a day in addition to
breastfeeding. It must be remembered that inadequate feeding of infants and young
children during the first two years is the main cause of malnutrition.
3.3.8 Continued Breastfeeding
Breastfeeding must be continued upto the age of two years or beyond. Continuing
breastfeeding while giving adequate complementary foods to the baby provides
all the benefits of breastfeeding to the baby. In other words, the child gets energy,
high quality protein, vitamin A, anti-infective properties and other nutrients besides
achieving emotional satisfaction from the breastfeeding much needed for
optimum development of the child. Breastfeeding especially at night ensures
sustained lactation. In the beginning when the complementary foods are
introduced after six months of age, the complementary food should be fed
when the infant is hungry. As the child starts taking complementary foods well,
the child should be given breastfeeding first and then the complementary food.
This will ensure adequate lactation.
3.3.9 Active Feeding
Adopting caring attitude while feeding the baby like talking to the child,
playing with the child stimulates appetite and development. One-two year
old child should be given food on a separate plate and encouraged to eat on
its own. Eating at the same time and at the same place also helps in improving
appetite and avoids distractions.
Optimal IYCF practices
a) Early initiation of breastfeeding; immediately after birth, preferably within
one hour.
b) Exclusive breastfeeding for the first six months of life i.e. 180 days (no
other foods or fluids, not even water; but allows infant to receive ORS,
drops, syrups of vitamins, minerals and medicines when required).
c) Timely introduction of complementary foods (solid, semisolid or soft
foods) after the age of six months i.e. 180 days.
d) Continued breastfeeding for 2 years or beyond.
e) Age appropriate complementary feeding for children 6–23 months, while
continuing breastfeeding. Children should receive food from 4 or more
food groups mentioned below and fed for a minimum number of times
(2 times for breasted infants 6–8 months; 3 times for breastfed children
9–23 months; 4 times for non-breastfed children 6–23 months).
i) Grains, roots and tubers, legumes and nuts;
ii) Dairy products;
iii) Flesh foods (meat fish, poultry);
iv) Eggs,
v) Vitamin A rich fruits and vegetables;
vi) Other fruits and vegetables
f) Active feeding for children during and after illness.
Feeding during illness
• Never starve the child.
• Feed energy-rich cereals-pulse diet with milk and mashed vegetables.
• Feed small quantities at frequent intervals.
• Continue breastfeeding as long as possible.
• Give plenty of fluids during illness.
• Use oral rehydration solution to prevent and correct dehydration during
diarrhea episod
Check Your Progress 1 Adolescent and Elderly
1) Breastfeeding should be started _____ hours after birth:
(a) Within 1 hour (b) 2 hours (c) 24 hours (d) 48 hours
2) Exclusive breastfeeding is sufficient for ____ months afterbirth:
(a) 1 month (b) 2 months (c) 6 months (d) 9 months
3) All are true of colostrum except:
a) Rich in proteins and minerals
b) Rich in anti-infective factors
c) Rich in fats
d) Secreted for first few days
4) True regarding complementary feeding one of the following is
a) Be initiated from 4 month onwards
b) Food from 4 or more food groups be given
c) Should be given twice a day to all children irrespective of their age
d) Need not continue breastfeeding after initiation of complementary feeds
5) True regarding complementary feeding is (Check all that apply)
a) Safe
b) Home-made
c) Liquid in nature
d) Timely
e) Adequate
3.4 NUTRITIONAL NEEDS OF CHILDREN AND
ADOLESCENTS
Childhood and adolescence are periods of continuous growth and development.
An infant grows rapidly, doubling its birth weight by 5 months and tripling it by
1 year of age. During the second year, the child increases not only in height by
7–8 cm but also gains 4 times of its birth weight. During the pre-adolescent
period the child grows, on an average, 6–7 cm in height and 1.5 to 3 kg in weight
every year and simultaneously development and maturation of various tissues
and organs take place. Children require more food as compared to adults. This is
because the children not only need food for maintaining the BMR, thermogenesis,
repairing wear and tear, but also for the important function of continuous growth.
Child therefore needs all kinds of extra nutrients, namely, proteins, fats
carbohydrates, minerals and vitamins.
Adolescent period (teenage) is spread almost over decade. It is characterised by
rapid increase in height and weight, hormonal changes, sexual maturation and
wide swings in emotion. Adolescent growth spurt starts at about 10–12 years in
girls and two years later in boys. The annual peak rates for height and weight are
9–10 cm and 8–10 kg. Development of critical bone mass is essential during this
period as this forms the ground for maintaining mineral integrity of the bone in
later life. The pattern and proportion of various body components like body water,
muscle mass, bone and fat increase during the entire childhood and adolescence
to reach adult values by about 18 years. Adolescent girls are at greater physiological
stress than boys because of menstruation. Their nutritional needs are of particular
importance as they have to prepare for motherhood. All these rapid anabolic
changes require more nutrients per unit body weight.
Growing children and adolescents require more calcium. Though recommended
dietary allowances for calcium are about 600–800 mg/day, it is desirable to give
higher quantities of calcium for adolescents to achieve high peak bone mass. To
achieve optimal peak bone mass, it is recommended to consume calcium rich
foods like milk and milk products, fox tail millet (Ragi), til etc.
Older children and adolescents should consume plenty of milk to fulfill the high
calcium requirements. Cooking oils/ghee (25–50 g) should be consumed. Over
indulgence in fats may be avoided. Excessive salt intake should be avoided
particularly by children having a family history of hypertension. Adolescence is
the vulnerable stage for developing wrong food habits as well as bad habits like
smoking, chewing tobacco or drinking alcohol. These should be avoided. In
addition to consumption of a nutritious well balanced diet, appropriate lifestyle
practices and involvement in physical activity such as games/sports should be
encouraged among children and adolescents.
Protein and Energy requirements
Based on the FAO/WHO recommendations the energy and protein requirements
are worked out for Indian children. These are given in Tables below 3.1 and 3.2.
Table 3.1 : Daily Energy Requirements for Children and Adolescents
Age (years) Boys (kcal/kg) Girls (kcal/kg)
1-3 1287 1193
4-6 1752 1630
7-9 2075 1833
10-12 2194 1965
13-15 2447 2056
16-18 2642 2064
Table 3.2 : Daily Protein Requirements of Children
Age (years) Boys (g/kg body weight) Girls (g/kg body weight)
1-2 1.81 1.81
2-3 1.67 1.67
3-4 1.61 1.61
4-6 1.52 1.52
7-9 1.48 1.48
10-12 1.46 1.45
13-15 1.4 1.33
16-18 1.31 1.21
73
Nutrition for Infant, Child,
Adolescent and Elderly
Check Your Progress 2
1) True regarding dietary requirement during adolescence is
a) Requirement is similar to adults
b) Daily protein requirement is 1gm/kg/day
c) Desirable fat intake of 20 gm/day
d) Over indulgence in fats may be avoided
2) True regarding dietary requirement of children is
a) Requirement is similar to adults
b) Fatty foods should be avoided
c) Daily protein requirement is 1gm/kg/day
d) Calcium requirement is increased
3) True regarding adolescent girls is
a) Requirement is similar to adolescent boys
b) More physiological stress compared to boys
c) Daily protein intake should be doubled
d) Growth spurt is 12–14 years of age
Fat Requirements
The minimum visible fat intake would also be 5% of total energy. For their
energy intake of 2400 kcal, minimum visible fat intake works out to 12 g/day,
but the desirable intake levels should be 20 g/day, which helps to reduce the
bulk of diet. Blanew diet for infants, children and adoliscents in shown in Table
3.3.
Table 3.3 : Balanced Diet for Infants, Children and Adolescents (Number of Portions)
Food Groups g/portion Infants 1 - 3 4 - 6 7 - 9 Years
6 - 12 yr yr yr 10 - 12 13 - 15 16 - 18
Months Girls Boys Girls Boys Girls Boys
Cereals & millets 30 0.5 2 4 6 8 10 11 14 11 15
Pulses 30 0.25 1 1.0 2 2 2 2 2.5 2.5 3
Milk (ml) & milk 100 4 5 5 5 5 5 5 5 5 5
products
Roots & tubers 100 0.5 0.5 1 1 1 1 1 1.5 2
Green leafy 100 0.25 0.5 0.5 1 1 1 1 1 1 1
vegetables
Other vegetables 100 0.25 0.5 1 1 2 2 2 2 2
Fruits 100 1 1 1 1 1 1 1 1 1 1
Sugar 5 2 3 4 4 6 6 5 4 5 6
Fat/ oil (visible) 5 4 5 5 6 7 7 8 9 7 10
Nutrition 3.5 NUTRITIONAL NEEDS OF PREGNANT AND
LACTATING MOTHERS
We have discussed nutritional needs of pregnant and lactating mother in details
in Unit 2. Let us read in brief over here as given below:
3.5.1 Nutrition of Pregnant Women
A pregnant woman needs:
• An adequate nutritious diet
• Adequate rest during last trimester
• Iron and Folic Acid tablets throughout the pregnancy
• Immunisation
Diet
• Increase food intake. A pregnantmother requires 300 extra calories per day
to meet the demands of pregnancy.
• Whole gram, pulses and legumes, sprouted pulses, leafy vegetables, jaggery,
dates, groundnuts are foods of plant origin having good iron content.
• Include green leafy vegetables in daily diet right from the beginning as
all foliage provide “folic acid” much needed during early months.
• Consume one seasonal fruit daily.
• Milk, curd, butter milk, egg, meat, fish are helpful.
• Iodised salt should be consumed as pregnant women requires sufficient
iodine for brain development of the child in the womb.
• Take plenty of fluids/water.
• Take small and frequent meals.
Rest
• Heavy work should be avoided throughout the pregnancy.
• Rest (in lying down position) during third trimester is important to enable
adequate flow of nutrients from mother to the child.
• A woman should gain 10–12 kg weight during pregnancy.
Iron and Folic Acid tablets
• IFA tablets should be consumed throughout the pregnancy.
• Iron tablets may cause black stools which are harmless.
• Iron and folic acid tablets prevent anaemia and helps a women to deliver
a normal healthy baby.
• The folic acid deficiency can cause “Neural tube defects” in the newborns.
Immunisation
Immunisation of the pregnant woman with tetanus toxoid (TT) given between
the 5th and 8th months of pregnancy in two doses at an interval of 4 weeks is
essential.